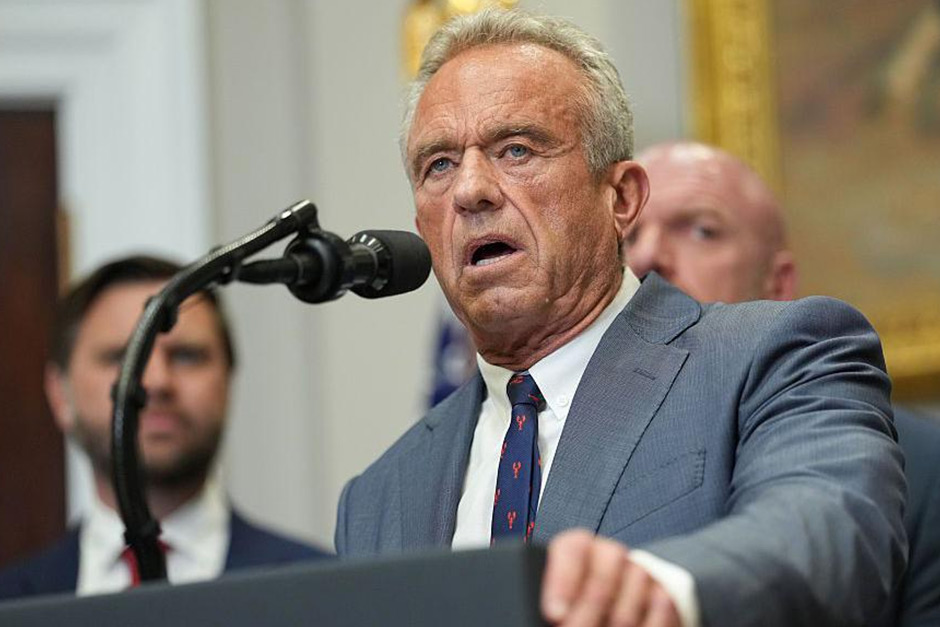
The murmurs of concern surrounding an infant vaccine study linked to Robert F. Kennedy Jr. in Africa have grown into a roar of criticism, yet recent news confirms a surprising persistence: the U.S. government states the study is still on. This isn’t merely an administrative update; it’s a flashpoint in a larger, complex conversation surrounding vaccine science, research ethics, and the fundamental responsibility owed to vulnerable populations.
The Unfolding Controversy: A Deep Dive into the Debate
The study, reportedly targeting infants in an African nation, has ignited a significant backlash from various corners of the scientific and ethical communities. Critics point to RFK Jr.’s well-documented history of vaccine skepticism, raising profound red flags about the methodology, intent, and potential for misinterpretation of findings. Such concerns are amplified by the very nature of vaccine research, where rigorous controls and unbiased scientific principles are absolutely paramount for public trust and safety.
Moreover, the choice of location – Africa – immediately brings to mind historical concerns about research conducted on vulnerable populations, where issues of informed consent, exploitation, and equitable benefit distribution are tragically familiar. The scientific community has largely expressed alarm, emphasizing the critical need for transparent, unbiased research, especially concerning infants and life-saving interventions. As Dr. Anya Sharma, a bioethicist, recently put it, “When studies involve vulnerable populations, the scrutiny must be tenfold. We cannot afford to compromise trust or ethical principles for any research, especially when public health is at stake.” The fear is not just about the immediate findings of the study, but the precedent it might set or the misinformation it could inadvertently fuel within an already polarized global health landscape.
Navigating the Official Stance: What Does “Still On” Really Mean?
So, what does it truly signify when the U.S. government says the study is “still on”? This is a statement that requires careful parsing. It doesn’t necessarily imply endorsement, funding, or active support from the U.S. government for RFK Jr.’s initiative. Instead, it often refers to the administrative reality that if a privately initiated study adheres to the regulatory frameworks and ethical guidelines of the host country, it can proceed. The U.S. government’s role, in such a context, is typically to ensure that American citizens or organizations operating abroad comply with relevant international and local laws, rather than to micromanage or halt private research unless there are clear breaches of ethical guidelines that fall under their direct jurisdiction.
This position highlights a delicate balance between respecting the sovereignty of other nations, facilitating private enterprise, and upholding global ethical research standards. It’s less an approval and more an acknowledgment of procedural ongoingness, leaving many to wonder about the extent of oversight and the implications of what could be perceived as a hands-off approach to deeply controversial research.
The Ripple Effect: Trust, Ethics, and Global Health
This controversy isn’t just about one study; it’s a stress test for the entire ecosystem of global health research. The persistent questions surrounding the study risk eroding public trust in scientific institutions and vaccine initiatives, especially in regions that have historically been exploited. It forces a broader conversation about who funds, conducts, and oversees research, particularly when the proponents have a controversial public profile and a history of challenging established medical consensus.
The stakes are incredibly high: ensuring that medical advancements are built on a foundation of unimpeachable ethics and transparent scientific practice. Any perceived ethical shortcuts or lack of robust oversight can have long-lasting consequences, making populations hesitant to participate in future, genuinely beneficial public health programs. This situation serves as a stark reminder that the battle for sound science and public health isn’t always fought in laboratories; it’s also waged in the arenas of public discourse, ethical review, and policy interpretation.
As this study purportedly continues, the global community will undoubtedly remain vigilant, scrutinizing its process and conclusions. The ramifications extend far beyond its immediate findings, impacting trust in science and potentially shaping global health efforts for years to come.