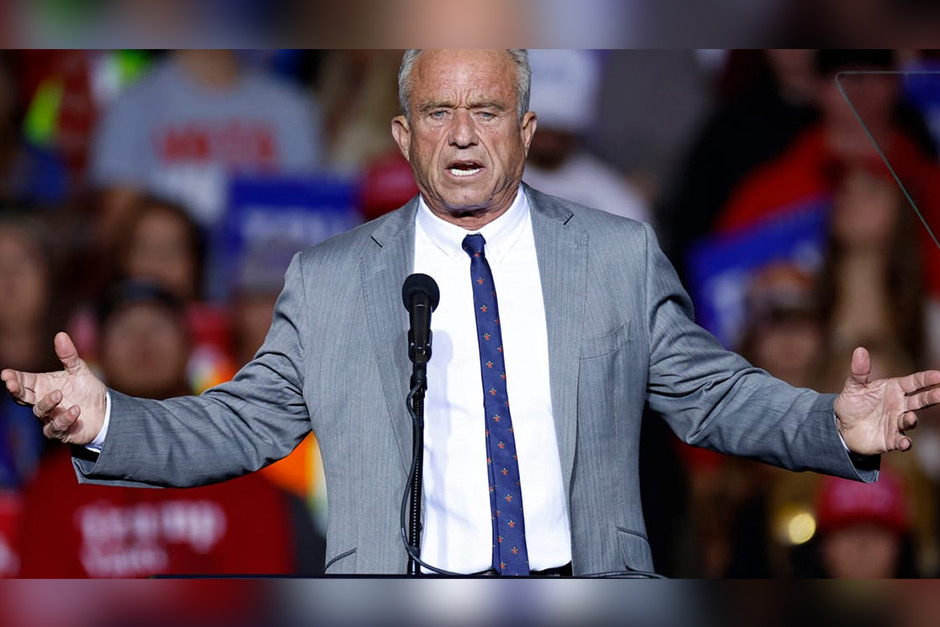
A recent proposal by Robert F. Kennedy Jr. suggests a significant pivot in U.S. vaccine policy, advocating for the nation to align more closely with European regulatory and purchasing models. While the idea of international harmonization might sound appealing, experts are flagging a critical potential consequence: such a shift could inadvertently lead to a substantial reduction in the number of vaccine doses available to Americans.
Emulating the European Model
RFK Jr.’s vision often points to European nations as a benchmark for various public health strategies, including those pertaining to vaccines. What does mimicking Europe entail in this context? It generally implies adopting different regulatory approval processes, potentially stricter manufacturing standards, and alternative procurement methods compared to the U.S.’s established framework. These European models often prioritize different aspects, sometimes focusing on slower, more deliberate approval pathways or centralized purchasing agreements that might differ vastly from the bulk buying and rapid deployment strategies historically employed by the United States.
Proponents of aligning with European systems often highlight perceived benefits such as enhanced transparency, different safety review protocols, or a more consolidated approach to public health procurement across a continent. However, translating these frameworks directly to the U.S. system, with its unique market dynamics, population size, and existing industrial infrastructure, presents a complex challenge.
The Supply Chain Squeeze
The core concern about fewer doses for Americans stems from several practical realities. The U.S. has, for decades, built a pharmaceutical ecosystem tailored to its own regulatory body, the FDA, and its unique market demands. This includes significant domestic manufacturing capabilities and supply chain partnerships optimized for rapid response and high volume under existing U.S. rules.
A sudden pivot to European standards could disrupt this delicate balance. Different regulatory hurdles mean manufacturers would need to reallocate resources, retool production lines, or even undergo entirely new approval processes. This isn’t a quick fix; it involves considerable time and investment, potentially delaying the rollout of new vaccines or even impacting the consistent supply of existing ones. Furthermore, the U.S. has often leveraged its economic power to secure large advance purchase agreements, ensuring priority access to innovative vaccines. If the U.S. adopts European-style procurement, it could find itself competing more directly with other nations for a global supply that wasn’t initially designed with a singular European-American standard in mind.
“We might see a situation where American manufacturers, suddenly beholden to entirely new regulatory frameworks or sourcing mandates, would face significant delays in delivering products to the American public,” notes Dr. Lena Khan, a public health policy analyst. “Shifting established gears in such a critical industry could inadvertently create bottlenecks and reduce overall availability, especially during times of high demand or emerging health crises.”
Balancing Ideals with Practicalities
The discussion around mimicking Europe on vaccines brings into sharp focus the tension between policy ideals and logistical realities. While there’s a compelling argument for learning from international partners and striving for best practices, the practical implications of a dramatic policy overhaul in a sector as critical as public health cannot be underestimated. The U.S. pharmaceutical landscape is vast and complex, designed to serve a population exceeding 330 million people.
Any move to adopt foreign models must carefully consider the potential for disruption to domestic supply chains, the impact on manufacturing output, and ultimately, how it would affect access for the average American. The goal of any vaccine policy should ideally be to ensure reliable, equitable, and sufficient access for all citizens, and any proposed change must be rigorously vetted against this core objective.
Ultimately, while the desire to improve and evolve public health strategies is commendable, a direct mirroring of European vaccine policies without careful consideration of the U.S.’s unique context could have unintended consequences, most notably in the form of fewer available doses when Americans need them most. The conversation underscores the intricate balance required to navigate global health standards while safeguarding national supply and public well-being.