The arrival of a newborn brings with it a flurry of preparations, decisions, and established routines, not least among them the schedule for vital immunizations. For decades, one of the first vaccinations a baby would receive was the hepatitis B shot, often administered within hours or days of birth. This practice has been a cornerstone of infant health, designed to protect against a potentially severe liver infection.
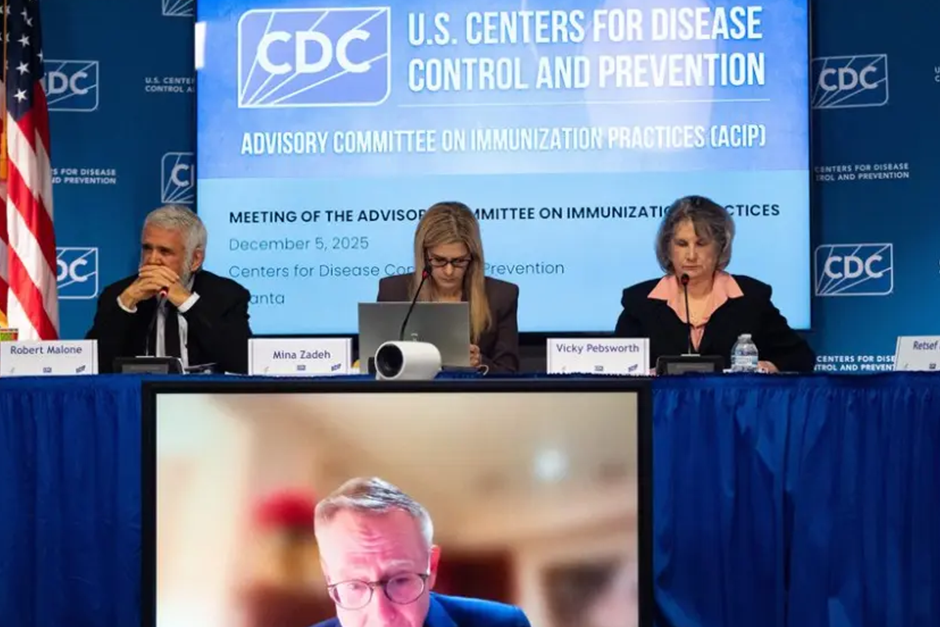
However, recent discussions among US vaccine advisers have brought a nuanced perspective to this long-standing guideline. The conversation centers not on the importance of the hepatitis B vaccine itself, but on the precise timing of that initial dose for every single baby. This shift highlights an evolving understanding of risk assessment and tailored medical advice.
The Foundational Role of the Hepatitis B Vaccine at Birth
For many years, the immediate administration of the hepatitis B vaccine to newborns has been a standard of care globally. The primary reason for this rapid deployment is to prevent perinatal transmission—the passing of the virus from a hepatitis B-infected mother to her baby during birth. Infants who contract hepatitis B at birth face a very high risk of developing chronic infection, which can lead to serious liver problems later in life, including cirrhosis and liver cancer.
Given that some mothers may be unaware of their hepatitis B status, or that test results might not be immediately available at the time of delivery, universal vaccination at birth served as a critical safety net. It ensured that all infants received a foundational layer of protection against a potentially silent but dangerous threat, effectively closing a significant pathway for transmission.
Introducing a Nuance: When Timing Can Be Flexible
The recent advisory suggests that for a specific subset of newborns, the immediate birth dose of the hepatitis B vaccine might not be strictly necessary. This nuance applies to infants born to mothers who are known to be hepatitis B negative and are considered low-risk for acquiring the infection during pregnancy. In these particular cases, where comprehensive maternal screening has confirmed the absence of hepatitis B, the immediate risk of perinatal transmission is virtually nonexistent.
For these babies, the first dose of the hepatitis B vaccine could potentially be delayed, perhaps given later as part of the routine childhood immunization schedule, typically around 1 or 2 months of age, or even up to 6 months depending on the specific schedule. It’s crucial to understand that this is not a recommendation to skip the vaccine entirely. The hepatitis B vaccine remains a vital protection for all children; rather, it’s an adjustment in the timing for a carefully defined group.
“It’s about precision public health,” remarked Dr. Elena Ramirez, a pediatrician specializing in infectious diseases. “For mothers who’ve been thoroughly screened and are negative, delaying that initial dose doesn’t put the baby at undue risk and can streamline the vaccine schedule for some families, without compromising essential protection.“
What This Means for Parents
This evolving guidance underscores the importance of personalized medical advice. For expectant parents, understanding your hepatitis B status through prenatal screening is paramount. Your healthcare provider will use this information, along with other risk factors, to determine the most appropriate vaccination schedule for your newborn.
If you are hepatitis B negative and considered low-risk, discussing the timing of your baby’s first hepatitis B shot with your pediatrician can help you understand the options. Conversely, if your hepatitis B status is unknown, or if you are hepatitis B positive, the recommendation for the immediate birth dose remains critically important to safeguard your baby’s health. In these situations, additional measures, such as hepatitis B immune globulin (HBIG), might also be administered to provide immediate, short-term protection.
Conclusion
The discussion around the timing of the hepatitis B vaccine at birth reflects the dynamic nature of medical science and public health recommendations. It’s a testament to continuous research and the aim to refine guidelines to best serve individual needs while maintaining robust public health safeguards. While the core message remains that the hepatitis B vaccine is essential for children, the recent advisory offers flexibility in timing for a specific group of newborns based on comprehensive maternal screening. As always, consulting with your healthcare provider is the best way to ensure your child receives the most appropriate and timely care.