In the complex tapestry of human health, the microscopic world within our gut holds profound sway. For millions worldwide, inflammatory bowel diseases (IBD), particularly ulcerative colitis (UC), represent a significant challenge, characterized by chronic inflammation of the large intestine. While the exact causes of UC have long remained elusive, a groundbreaking new study sheds light on a potential microbial culprit, suggesting that a specific bacterium might ignite the very first stages of the debilitating condition.
Published in a leading scientific journal, this research offers a crucial piece to the intricate puzzle of UC pathogenesis. For countries like India, where lifestyle changes and improved diagnostics are revealing a rising incidence of IBD, understanding these early triggers could pave the way for more effective prevention and intervention strategies, potentially transforming patient care.
Unravelling the Microbial Link: The Bilophila Wadsworthia Hypothesis
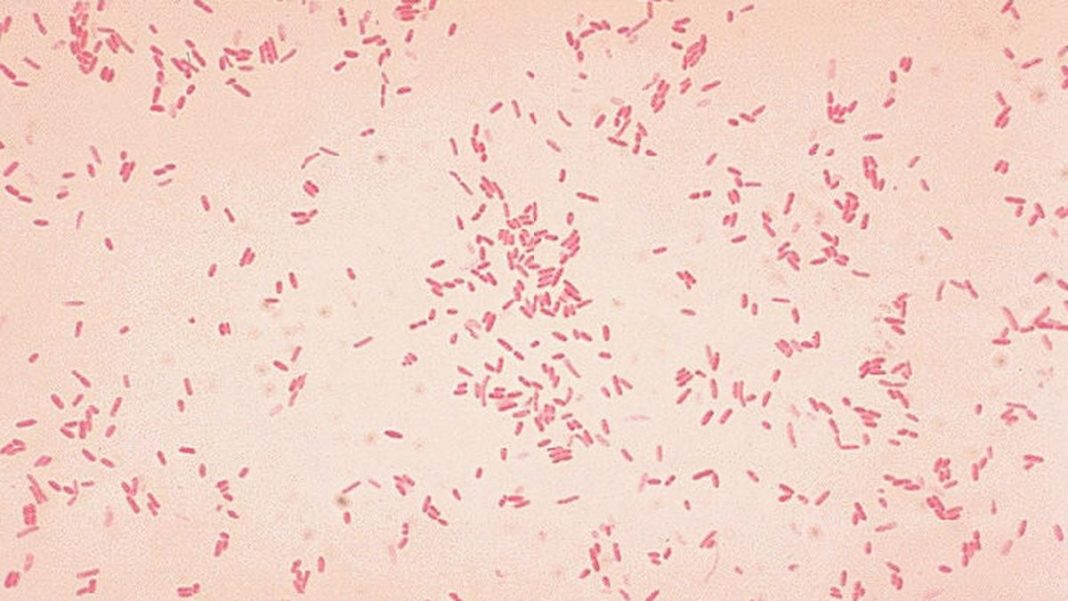
The study meticulously investigated the role of a bacterium known as Bilophila wadsworthia. This microbe, often found in the gut, is known for its ability to produce hydrogen sulfide – a gas that, in small amounts, plays a role in various bodily functions, but in excess, can be toxic and inflammatory. The researchers, through a series of sophisticated experiments involving both animal models and human tissue samples, discovered a compelling correlation.
Their findings indicate that an elevated presence of Bilophila wadsworthia, and consequently increased hydrogen sulfide production, could be directly linked to the initiation of inflammation in the colon lining. This isn’t just about the presence of the microbe; it’s about its metabolic activity creating an environment hostile to the delicate intestinal barrier. The study suggests that this bacterium, by damaging the protective mucus layer and compromising the integrity of epithelial cells, could set the stage for the chronic inflammation characteristic of UC, long before clinical symptoms become apparent.
What makes this research particularly significant is its focus on the “first stages” of the disease. While many studies have looked at the microbial communities in established UC, this work delves into the initial spark, offering a potential window for early intervention. Understanding what triggers inflammation at such a fundamental level could redefine how we approach diagnosis and treatment.
Implications for Diagnosis and Treatment in India
The insights garnered from this study hold immense promise, particularly for the Indian healthcare landscape. The burden of UC, though historically considered lower than in Western countries, is undeniably on the rise in India, influenced by factors such as dietary shifts, urbanization, and improved diagnostic capabilities. Early and accurate diagnosis remains a challenge, often leading to delayed treatment and more severe disease progression.
If Bilophila wadsworthia indeed plays a pivotal role in early inflammation, it opens several exciting avenues. Firstly, it could lead to the development of novel diagnostic biomarkers. Imagine a future where a simple gut microbiome analysis could flag individuals at risk for UC, enabling proactive measures before the disease takes hold. Secondly, and perhaps more profoundly, it points towards targeted therapeutic strategies.
Rather than merely managing symptoms, future treatments could focus on modulating the gut microbiome. This might involve dietary interventions specifically designed to limit the growth of Bilophila wadsworthia or to neutralize its harmful byproducts. Probiotics or prebiotics tailored to restore microbial balance could also become a key part of the therapeutic arsenal. Furthermore, the development of specific antimicrobial agents targeting this bacterium, or even compounds that neutralize excess hydrogen sulfide, could represent a paradigm shift in UC management.
“This study is a significant leap forward in understanding ulcerative colitis, particularly for a country like India where we are seeing an increasing incidence,” states Dr. Anjali Sharma, a leading gastroenterologist based in Mumbai. “Identifying a potential microbial trigger for the early stages offers us the hope of developing preventative strategies and personalized interventions. Imagine being able to intervene even before a patient develops full-blown symptoms – that would be revolutionary for patient quality of life and healthcare burden.”
The potential to identify and address the root cause, rather than just the symptoms, could drastically improve patient outcomes, reduce the need for invasive surgeries, and alleviate the significant economic and emotional strain associated with chronic UC.
Charting the Future: From Research to Clinical Practice
While the findings are compelling, it is crucial to remember that this study represents a foundational step. Further research is undoubtedly needed to validate these findings in larger human cohorts and to fully understand the intricate interactions between Bilophila wadsworthia, other gut microbes, host genetics, and environmental factors that collectively contribute to UC. Clinical trials will be essential to translate these microbial insights into tangible patient benefits.
Nevertheless, this new understanding of Bilophila wadsworthia‘s potential role in sparking the first stages of ulcerative colitis is a beacon of hope. It underscores the critical importance of our gut microbiome in health and disease and opens up exciting possibilities for precision medicine in the fight against IBD. For individuals in India and globally, this microbe’s might, once understood, could become a key to unlocking better health and a future free from the debilitating grip of ulcerative colitis.
The journey from a laboratory discovery to a widespread clinical application is often long, but with each groundbreaking study like this, we move closer to a deeper understanding and more effective treatments for complex diseases, bringing renewed hope to millions.