In a nation grappling with a significant burden of respiratory illnesses, certain conditions often lurk beneath the surface, challenging diagnosis and effective management. Among these are Alpha-1 Antitrypsin Deficiency (AATD) and its significant link to a chronic lung condition known as bronchiectasis. While often overlooked, understanding this genetic predisposition is crucial for improving patient outcomes and alleviating the widespread impact of lung disease in India.
Alpha-1 Antitrypsin Deficiency: A Silent Genetic Threat
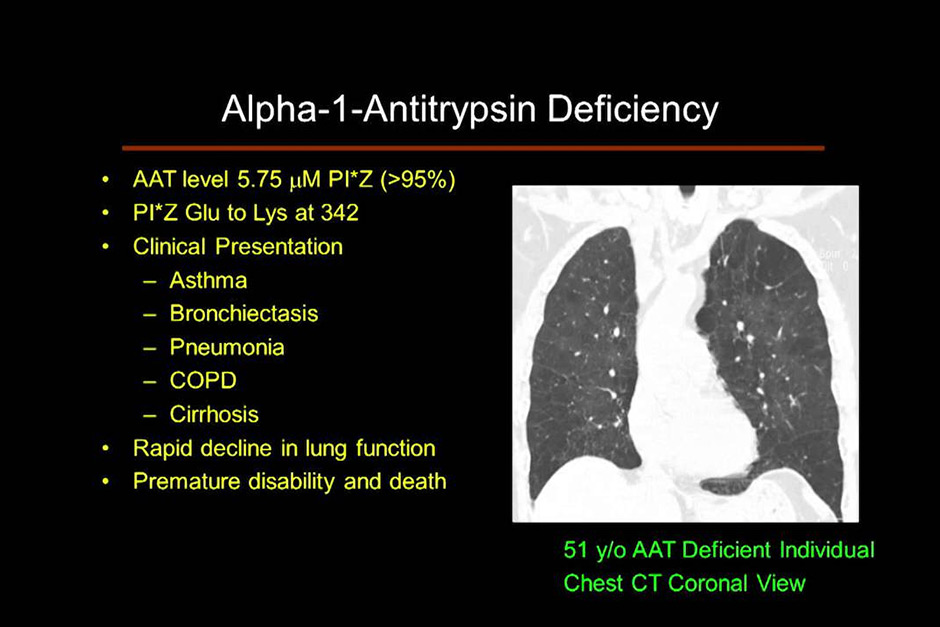
Alpha-1 Antitrypsin Deficiency is a genetic disorder characterised by low levels of alpha-1 antitrypsin (AAT), a protective protein primarily produced in the liver. AAT plays a vital role in shielding the lungs from inflammation and damage, particularly from an enzyme called neutrophil elastase. When levels of AAT are insufficient, this enzyme can go unchecked, leading to progressive destruction of lung tissue.
While AATD can manifest with liver disease, its most significant impact is often on the respiratory system, manifesting as early-onset emphysema or, critically, bronchiectasis. In India, the awareness and diagnosis of AATD remain notably low. Many patients present with symptoms mimicking more common conditions like asthma, COPD, or tuberculosis, leading to delayed or misdiagnosis. This delay is particularly concerning given the progressive nature of lung damage without proper intervention.
Bronchiectasis: Unravelling its Roots
Bronchiectasis is a chronic lung condition characterised by the irreversible widening and damage of the airways (bronchi). This damage leads to a buildup of mucus, making the lungs a fertile ground for recurrent bacterial infections and persistent inflammation. Patients often experience a chronic cough, production of thick sputum, shortness of breath, and frequent chest infections.
While various factors can cause bronchiectasis – including severe infections, cystic fibrosis, or immune deficiencies – AATD stands out as a primary underlying cause in a significant number of non-cystic fibrosis cases. In individuals with AATD, the ongoing elastase-mediated destruction of lung tissue weakens the bronchial walls, making them susceptible to dilation and permanent damage characteristic of bronchiectasis. The interplay is insidious: the genetic deficiency initiates damage, which then creates an environment prone to infection and inflammation, further worsening the bronchiectasis.
“The link between Alpha-1 Antitrypsin Deficiency and bronchiectasis is a critical piece of the diagnostic puzzle that we must emphasize more in Indian clinical practice,” says Dr. Priya Singh, a senior pulmonologist based in Delhi. “Many patients with unexplained bronchiectasis or early-onset emphysema could potentially have AATD, and timely diagnosis can alter their disease trajectory and management significantly. Without specific testing, these individuals often endure years of symptomatic treatment without addressing the root cause.”
Diagnosis and Management in the Indian Context
Diagnosing AATD typically involves a simple blood test to measure AAT levels, followed by genetic testing to identify specific mutations. Bronchiectasis is diagnosed using a high-resolution computed tomography (HRCT) scan of the chest. The challenge in India lies not only in physician awareness but also in the accessibility and affordability of these specialised tests, especially in smaller towns and rural areas.
Management of AATD-related lung disease often involves augmentation therapy, where purified human AAT is infused intravenously to supplement the deficient protein. While effective in slowing lung damage, this therapy is exceptionally expensive and not widely available or subsidised in India. Therefore, management often focuses on supportive care for bronchiectasis: aggressive chest physiotherapy, bronchodilators, antibiotics for infections, and vaccinations to prevent respiratory illnesses. Lifestyle modifications, such as smoking cessation, are also paramount.
Raising awareness among both healthcare professionals and the general public is the first crucial step. Integrating AATD testing into the diagnostic algorithm for patients with unexplained bronchiectasis, COPD, or early-onset emphysema could dramatically improve early detection. Furthermore, advocating for better access to genetic counselling and potentially affordable augmentation therapies for patients with AATD could transform the lives of many individuals and families affected by this often-misunderstood condition.
Understanding the interplay between Alpha-1 Antitrypsin Deficiency and bronchiectasis is more than just academic; it’s about empowering patients with accurate diagnoses and appropriate care. As India’s healthcare system evolves, recognising and addressing these nuanced genetic conditions will be key to fostering healthier lung outcomes nationwide.